Tackling cancer at the nanoscale
When Paula Hammond first arrived on MIT’s campus as a first-year student in the early 1980s, she wasn’t sure if she belonged. In fact, as she told an MIT audience yesterday, she felt like “an imposter.”
However, that feeling didn’t last long, as Hammond began to find support among her fellow students and MIT’s faculty. “Community was really important for me, to feel that I belonged, to feel that I had a place here, and I found people who were willing to embrace me and support me,” she said.
Hammond, a world-renowned chemical engineer who has spent most of her academic career at MIT, made her remarks during the 2023-24 James R. Killian Jr. Faculty Achievement Award lecture.
Established in 1971 to honor MIT’s 10th president, James Killian, the Killian Award recognizes extraordinary professional achievements by an MIT faculty member. Hammond was chosen for this year’s award “not only for her tremendous professional achievements and contributions, but also for her genuine warmth and humanity, her thoughtfulness and effective leadership, and her empathy and ethics,” according to the award citation.
“Professor Hammond is a pioneer in nanotechnology research. With a program that extends from basic science to translational research in medicine and energy, she has introduced new approaches for the design and development of complex drug delivery systems for cancer treatment and noninvasive imaging,” said Mary Fuller, chair of MIT’s faculty and a professor of literature, who presented the award. “As her colleagues, we are delighted to celebrate her career today.”
In January, Hammond began serving as MIT’s vice provost for faculty. Before that, she chaired the Department of Chemical Engineering for eight years, and she was named an Institute Professor in 2021.
A versatile technique
Hammond, who grew up in Detroit, credits her parents with instilling a love of science. Her father was one of very few Black PhDs in biochemistry at the time, while her mother earned a master’s degree in nursing from Howard University and founded the nursing school at Wayne County Community College. “That provided a huge amount of opportunity for women in the area of Detroit, including women of color,” Hammond noted.
After earning her bachelor’s degree from MIT in 1984, Hammond worked as an engineer before returning to the Institute as a graduate student, earning her PhD in 1993. After a two-year postdoc at Harvard University, she returned to join the MIT faculty in 1995.
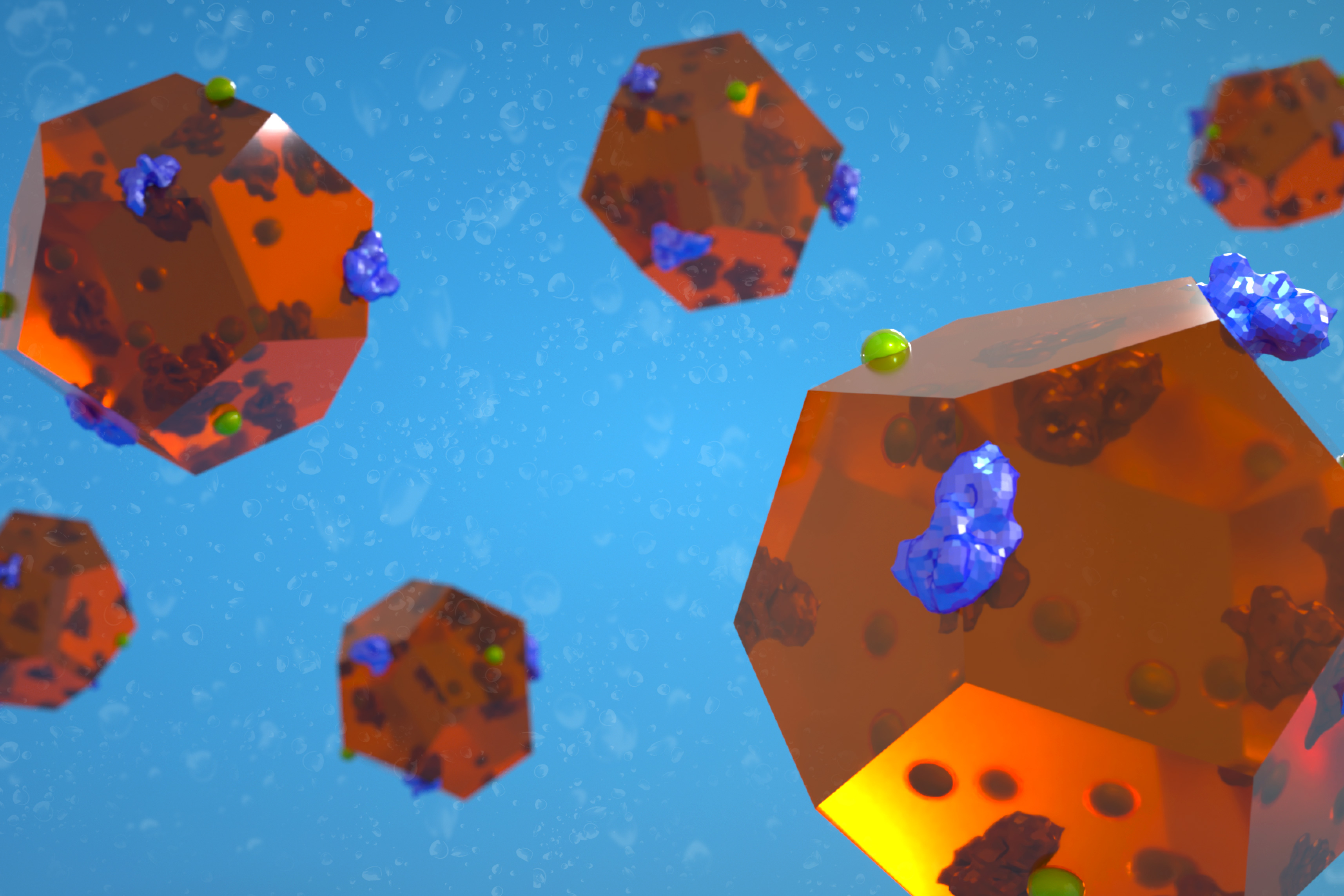
At the heart of Hammond’s research is a technique she developed to create thin films that can essentially “shrink-wrap” nanoparticles. By tuning the chemical composition of these films, the particles can be customized to deliver drugs or nucleic acids and to target specific cells in the body, including cancer cells.
To make these films, Hammond begins by layering positively charged polymers onto a negatively charged surface. Then, more layers can be added, alternating positively and negatively charged polymers. Each of these layers may contain drugs or other useful molecules, such as DNA or RNA. Some of these films contain hundreds of layers, others just one, making them useful for a wide range of applications.
“What’s nice about the layer-by-layer process is I can choose a group of degradable polymers that are nicely biocompatible, and I can alternate them with our drug materials. This means that I can build up thin film layers that contain different drugs at different points within the film,” Hammond said. “Then, when the film degrades, it can release those drugs in reverse order. This is enabling us to create complex, multidrug films, using a simple water-based technique.”
Hammond described how these layer-by-layer films can be used to promote bone growth, in an application that could help people born with congenital bone defects or people who experience traumatic injuries.
For that use, her lab has created films with layers of two proteins. One of these, BMP-2, is a protein that interacts with adult stem cells and induces them to differentiate into bone cells, generating new bone. The second is a growth factor called VEGF, which stimulates the growth of new blood vessels that help bone to regenerate. These layers are applied to a very thin tissue scaffold that can be implanted at the injury site.
Hammond and her students designed the coating so that once implanted, it would release VEGF early, over a week or so, and continue releasing BMP-2 for up to 40 days. In a study of mice, they found that this tissue scaffold stimulated the growth of new bone that was nearly indistinguishable from natural bone.
Targeting cancer
As a member of MIT’s Koch Institute for Integrative Cancer Research, Hammond has also developed layer-by-layer coatings that can improve the performance of nanoparticles used for cancer drug delivery, such as liposomes or nanoparticles made from a polymer called PLGA.
“We have a broad range of drug carriers that we can wrap this way. I think of them like a gobstopper, where there are all those different layers of candy and they dissolve one at a time,” Hammond said.
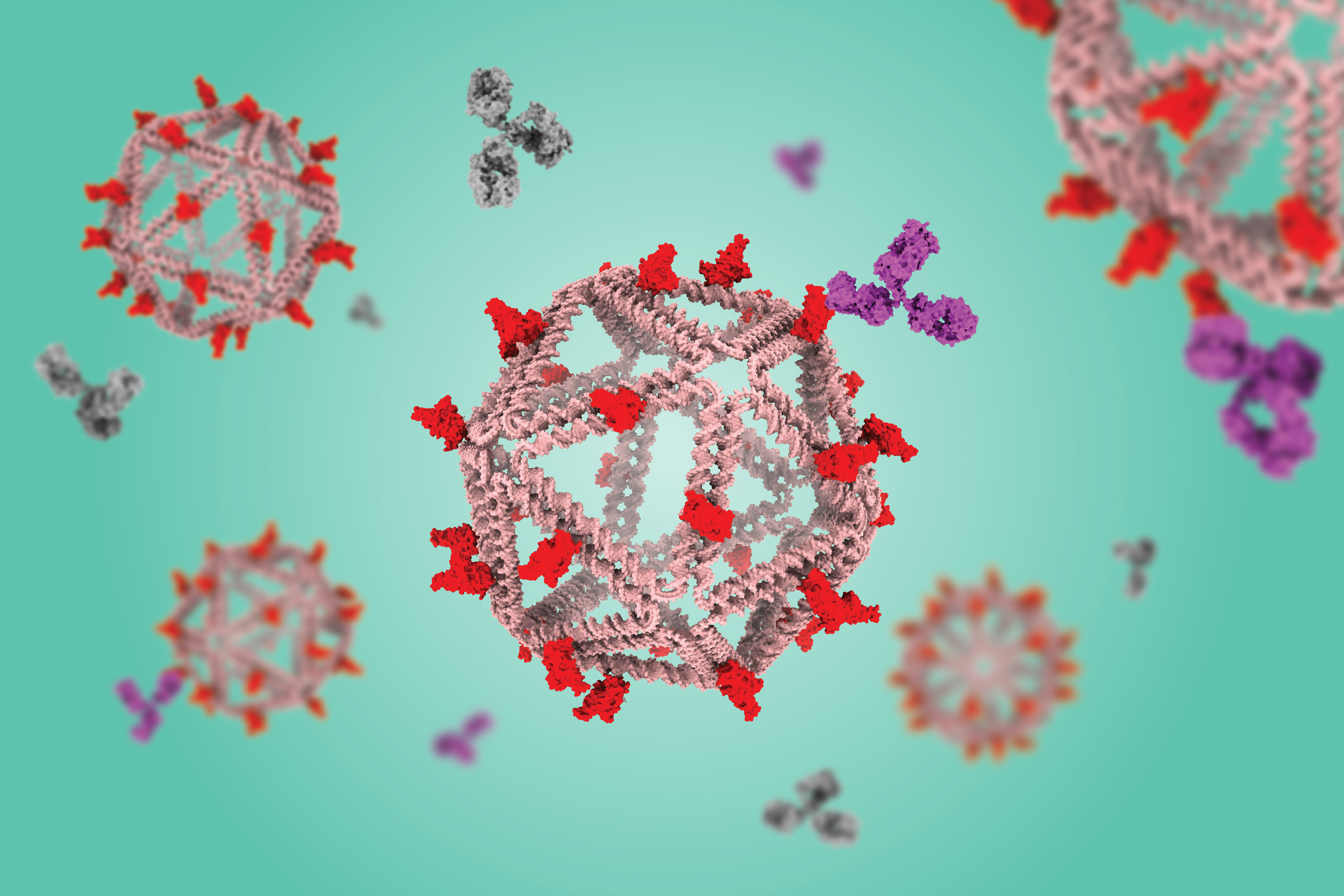
Using this approach, Hammond has created particles that can deliver a one-two punch to cancer cells. First, the particles release a dose of a nucleic acid such as short interfering RNA (siRNA), which can turn off a cancerous gene, or microRNA, which can activate tumor suppressor genes. Then, the particles release a chemotherapy drug such as cisplatin, to which the cells are now more vulnerable.
The particles also include a negatively charged outer “stealth layer” that protects them from being broken down in the bloodstream before they can reach their targets. This outer layer can also be modified to help the particles get taken up by cancer cells, by incorporating molecules that bind to proteins that are abundant on tumor cells.
In more recent work, Hammond has begun developing nanoparticles that can target ovarian cancer and help prevent recurrence of the disease after chemotherapy. In about 70 percent of ovarian cancer patients, the first round of treatment is highly effective, but tumors recur in about 85 percent of those cases, and these new tumors are usually highly drug resistant.
By altering the type of coating applied to drug-delivering nanoparticles, Hammond has found that the particles can be designed to either get inside tumor cells or stick to their surfaces. Using particles that stick to the cells, she has designed a treatment that could help to jumpstart a patient’s immune response to any recurrent tumor cells.
“With ovarian cancer, very few immune cells exist in that space, and because they don’t have a lot of immune cells present, it’s very difficult to rev up an immune response,” she said. “However, if we can deliver a molecule to neighboring cells, those few that are present, and get them revved up, then we might be able to do something.”
To that end, she designed nanoparticles that deliver IL-12, a cytokine that stimulates nearby T cells to spring into action and begin attacking tumor cells. In a study of mice, she found that this treatment induced a long-term memory T-cell response that prevented recurrence of ovarian cancer.
Hammond closed her lecture by describing the impact that the Institute has had on her throughout her career.
“It’s been a transformative experience,” she said. “I really think of this place as special because it brings people together and enables us to do things together that we couldn’t do alone. And it is that support we get from our friends, our colleagues, and our students that really makes things possible.”

© Photo: Jake Belcher