Nancy Kanwisher, Robert Langer, and Sara Seager named Kavli Prize Laureates
MIT faculty members Nancy Kanwisher, Robert Langer, and Sara Seager are among eight researchers worldwide to receive this year’s Kavli Prizes.
A partnership among the Norwegian Academy of Science and Letters, the Norwegian Ministry of Education and Research, and the Kavli Foundation, the Kavli Prizes are awarded every two years to “honor scientists for breakthroughs in astrophysics, nanoscience and neuroscience that transform our understanding of the big, the small and the complex.” The laureates in each field will share $1 million.
Understanding recognition of faces
Nancy Kanwisher, the Walter A Rosenblith Professor of Brain and Cognitive Sciences and McGovern Institute for Brain Research investigator, has been awarded the 2024 Kavli Prize in Neuroscience with Doris Tsao, professor in the Department of Molecular and Cell Biology at the University of California at Berkeley, and Winrich Freiwald, the Denise A. and Eugene W. Chinery Professor at the Rockefeller University.
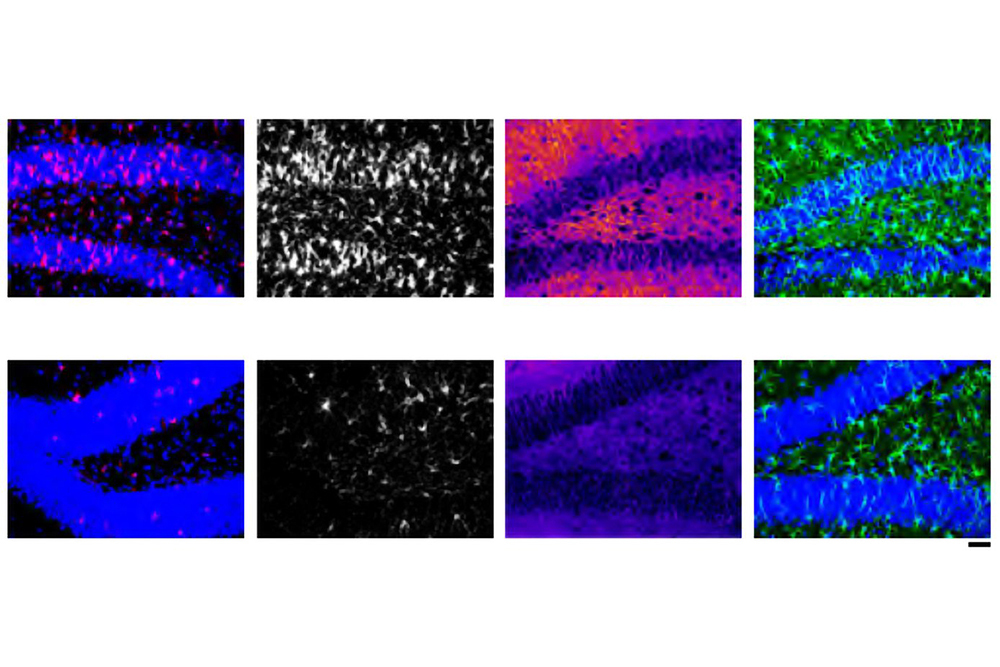
Kanwisher, Tsao, and Freiwald discovered a specialized system within the brain to recognize faces. Their discoveries have provided basic principles of neural organization and made the starting point for further research on how the processing of visual information is integrated with other cognitive functions.
Kanwisher was the first to prove that a specific area in the human neocortex is dedicated to recognizing faces, now called the fusiform face area. Using functional magnetic resonance imaging, she found individual differences in the location of this area and devised an analysis technique to effectively localize specialized functional regions in the brain. This technique is now widely used and applied to domains beyond the face recognition system.
Integrating nanomaterials for biomedical advances
Robert Langer, the David H. Koch Institute Professor, has been awarded the 2024 Kavli Prize in Nanoscience with Paul Alivisatos, president of the University of Chicago and John D. MacArthur Distinguished Service Professor in the Department of Chemistry, and Chad Mirkin, professor of chemistry at Northwestern University.
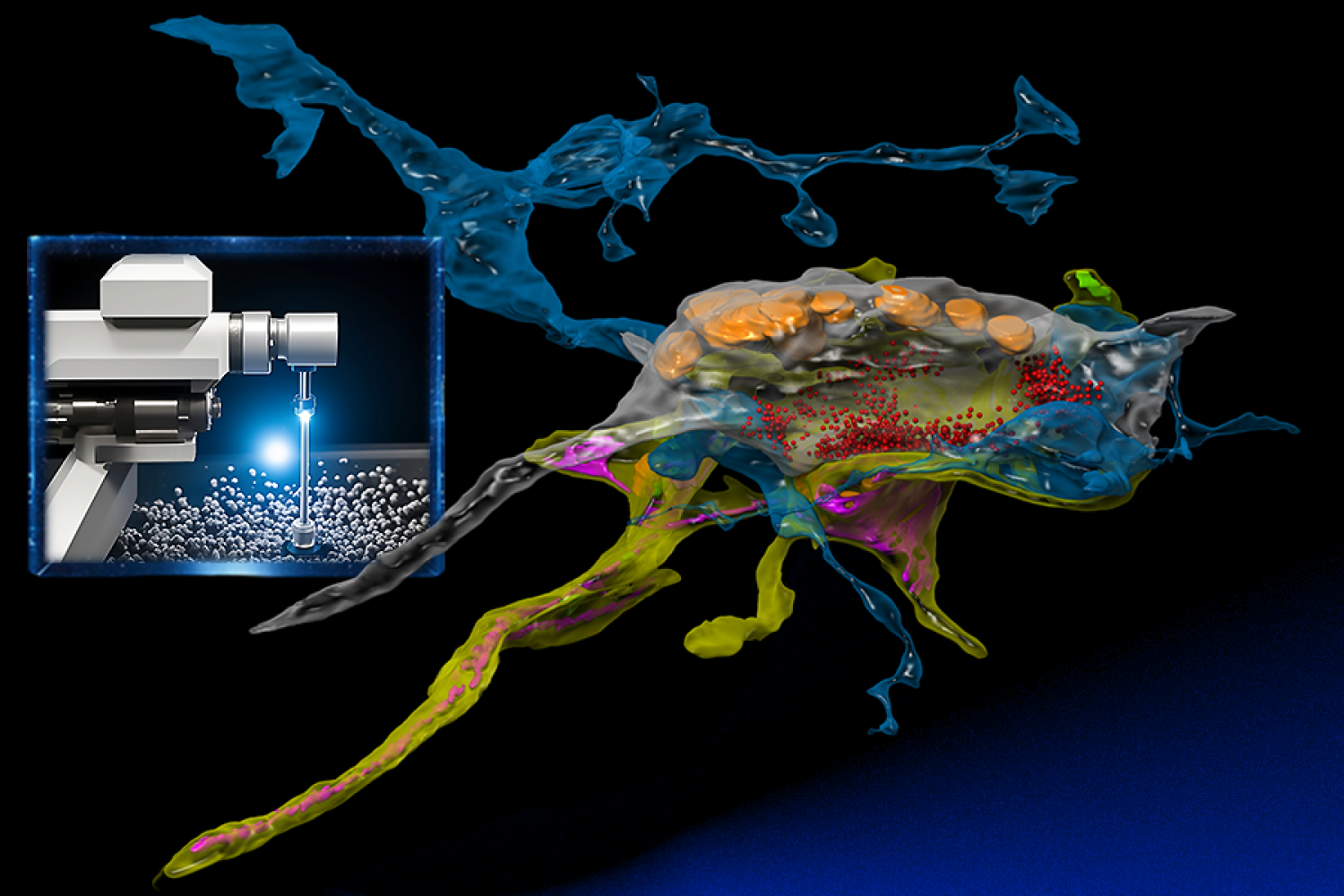
Langer, Alivisatos, and Mirkin each revolutionized the field of nanomedicine by demonstrating how engineering at the nano scale can advance biomedical research and application. Their discoveries contributed foundationally to the development of therapeutics, vaccines, bioimaging, and diagnostics.
Langer was the first to develop nanoengineered materials that enabled the controlled release, or regular flow, of drug molecules. This capability has had an immense impact for the treatment of a range of diseases, such as aggressive brain cancer, prostate cancer, and schizophrenia. His work also showed that tiny particles, containing protein antigens, can be used in vaccination, and was instrumental in the development of the delivery of messenger RNA vaccines.
Searching for life beyond Earth
Sara Seager, the Class of 1941 Professor of Planetary Sciences in the Department of Earth, Atmospheric and Planetary Sciences and a professor in the departments of Physics and of Aeronautics and Astronautics, has been awarded the 2024 Kavli Prize in Astrophysics along with David Charbonneau, the Fred Kavli Professor of Astrophysics at Harvard University.
Seager and Charbonneau are recognized for discoveries of exoplanets and the characterization of their atmospheres. They pioneered methods for the detection of atomic species in planetary atmospheres and the measurement of their thermal infrared emission, setting the stage for finding the molecular fingerprints of atmospheres around both giant and rocky planets. Their contributions have been key to the enormous progress seen in the last 20 years in the exploration of myriad exoplanets.
Kanwisher, Langer, and Seager bring the number of all-time MIT faculty recipients of the Kavli Prize to eight. Prior winners include Rainer Weiss in astrophysics (2016), Alan Guth in astrophysics (2014), Mildred Dresselhaus in nanoscience (2012), Ann Graybiel in neuroscience (2012), and Jane Luu in astrophysics (2012).

© Photos: Nils Lund